納米刀是一種新的腫瘤消融技術,它通過釋放高壓脈沖在腫瘤細胞上形成納米級永久性穿孔,破壞細胞內平衡,使細胞快速凋亡。納米刀在2010年3月通過了歐盟的CE認證,2011年10月獲美國FDA批准應用於臨床。截止到目前,全球已有一百多個腫瘤醫院采用了納米刀技術。

通過眾多臨床研究表明,納米刀是一種安全而又高效的腫瘤治療技術,與其他腫瘤治療技術相比,它具有以下優勢:
1. 消融時間短
治療直徑約3cm的實體腫瘤時,納米刀一般只需90個100毫秒的超短脈沖。一組治療時間不到一分鍾。因此即使有三個或四個相互重疊的消融區,全程的消融時間也不會超過5分鍾。

2. 治療區域的血管、神經等重要組織得以保留
納米刀消融技術的另一個特點是它能夠保護消融區內重要的組織結構。所有經過納米刀治療的肝組織中,其重要結構,如肝動脈,肝靜脈,門脈,肝內膽管均能得到良好的保護。納米刀是非熱能消融,不是以升溫或降溫的方式使蛋白質發生變性,各類蛋白質和DNA不會受到破壞,而可以得到修復。

3. 不受熱島效應影響
納米刀的消融主要是通過電脈沖擊穿細胞膜,在此過程中不會產生熱量,也不會受到其他外界溫度影響。
4. 治療徹底,治療邊界清晰
納米刀的另一個優勢是,無論腫瘤是靠近血管的,還是形狀不規則或者是大腫瘤,IRE都能對其進行消融。此外,納米刀消融區邊界清晰,劃界厚度僅為1-2細胞單元。去治療區和非治療區域涇渭分明,因此,對納米刀的有效性、治療結果以及後續跟蹤都能進行更准確的判斷和評估。

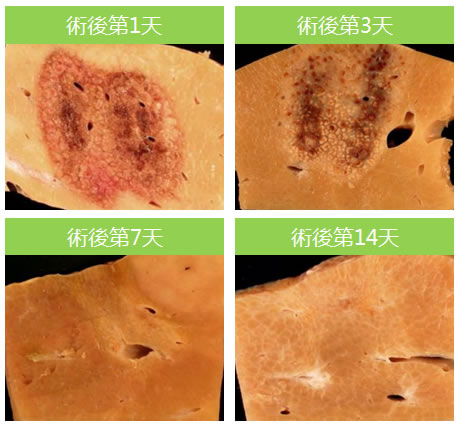
5. 治療區域可恢複正常功能
納米刀誘導腫瘤細胞出現凋亡。凋亡的優點之一就是它能夠利用免疫來促進細胞死亡,人體將把細胞凋亡識別為正常的細胞死亡過程,然後通過細胞吞噬作用將凋亡組織清除掉,促進正常組織的再生與修複。
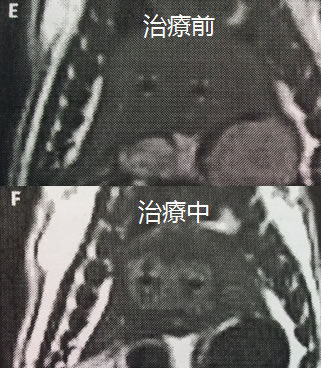
6. 效果過程可實時監控
納米刀治療能夠通過超聲、CT和MR進行影像導航和監控。在影像設備的輔助下,可以對納米刀探針的定位、標靶區域的消融過程以及最終消融區的大小進行實時監控,而且影像中消融區邊界的精確度可與組織學上的精確度相媲美。用超聲或CT監控到的消融區與病理分析中測量真實的消融區的尺寸偏差僅有幾毫米。由此可見,納米刀消融的影像監控的精確度非常高。影像中還能清楚顯示未消融的殘餘癌症細胞,於此醫生能夠對其再次進行消融。另外,實時監控還可以讓醫生觀察到消融區周圍組織的變化,從而推斷出並發症出現的可能性,保障病人的安全以及有助於其術後快速恢複。
7. 納米刀可適應更多複雜的病情
對於靠近大血管、膽管、胰管、肝門靜脈等危險區域的腫瘤,可以進行消融治療,以及對於前列腺腫瘤或者脊椎附近腫瘤,不會因為神經受損而發生癱瘓、性功能喪失等情況。所以相對來說,納米刀治療腫瘤是安全而有效的。
附:來源: Irreversible Electroporation (IRE) | University of Maryland Medical Center
Needle-like Probes Destroy Diseased Cells But Spare Healthy Tissue
IRE uses electrical energy to target tumors at the cellular level. Using short electrical pulses, IRE breaks open the tumor cell walls, causing these cancer cells to die1。
The key difference with IRE compared to other treatments is that this electrical field does not produce extreme heat or cold. It may selectively damage the cancerous cells, sparing healthy tissue and structures that may be nearby, allowing us to provide more targeted treatment1,Doctors create a precise electrical field by first mapping the tumor using state-of-the-art computed tomography (CT) technology. The interventional radiologists have a CT scanner in the treatment room, so they are able to make up-to-the minute calculations on the size and location of the tumor.
Once we determine the treatment area, we insert the electrode probes through the skin into the tumor, creating a field around the lesion. We then send short, intense electrical pulses - each less than 100 microseconds - between the probes, killing the tumor cells. Then the body's normal healing response takes over, naturally producing new cells and absorbing the cells that have been targeted2.
IRE is performed under general anesthesia. The time it takes to place the needles varies based on the size and location of the tumor. Because the procedure is considered to be minimally invasive, recovery time may be faster when compared to some other treatments, with some soreness from the needles themselves. There is little scarring because of the way IRE causes the cancer cells to open and die, taking advantage of the body's natural healing ability.
This procedure is another example of the commitment of University of Maryland faculty to bring cutting-edge technology to their patients, offering them another treatment option when traditional surgery may not be effective for their particular condition3.
IRE may be a viable alternative for patients with tumors in areas we call ”˜high-rent' zones, difficult-to-treat locations that may be near or touching a blood vessel, nerve or duct4。
1.Ziv Haskal, M.D., professor of diagnostic radiology and surgery at the University of Maryland School of Medicine
2.Fred Moeslein, M.D., Ph.D., assistant professor of diagnostic radiology and nuclear medicine at the University of Maryland School of Medicine, and interventional radiologist at the University of Maryland Medical Center.
3.E. Albert Reece, M.D., Ph.D., M.B.A., vice president for medical affairs at the University of Maryland and dean of the University of Maryland School of Medicine.
4.Rahul Patel, M.D., assistant professor of diagnostic radiology and nuclear medicine at the University of Maryland School of Medicine, and interventional radiologist at the University of Maryland Medical Center.
Prev: 納米刀的原理


 Follow on Facebook
Follow on Facebook Follow on Twitter
Follow on Twitter Subscribe to RSS
Subscribe to RSS